Age: 59
Hometown: Gastonia, N.C.
Surgeon: Dr. William Hunter
Indications: spondylolisthesis
Procedure: XLIF®
Surgery date: February 14, 2011
“I’m so grateful for Dr. Hunter for this miracle!” – Christine
Life prior to surgery:
Christine struggles with Lupis and constantly had health issues. Her back pain started gradually and started running down her legs. She underwent a spine surgery in 2002 for herniated disc. After this surgery, she was in extreme pain. It took Christine a whole year to get back to her “normal” lifestyle, and she was forced to walk with a cane. Over the subsequent years, she sought multiple consultations with surgeons who recommended conservative care. She tried epidurals for several years, but these failed to provide long-term pain relief. She experienced numbness and a burning sensation in her legs, which inhibited Christine’s ability to stand, walk or do any type of exercises. Christine was then referred to Dr. Hunter by a friend and sought a consultation. “The pain was completely affecting my life and I was tired of hurting and going back and forth between doctors. I couldn’t sleep at night because of the pain.” Dr. Hunter diagnosed her with disc degeneration. Dr. Hunter recommended the XLIF® procedure, and although she was fearful, her pain was so severe in her back and legs that she was willing to try anything for relief. “I felt like my legs were burning before surgery. It was so painful!”
Situation today:
Christine had XLIF® surgery on February 14, 2011. When she awoke from surgery, she was able to walk immediately! She was able to dress herself the morning after and returned home. She struggled with initial muscle spasms, which subsided quickly, and Christine didn’t have to take any pain pills. She was able to resume light household chores immediately. Christine was amazed at how quickly she was able to recover. She didn’t need the assistance of in-home physical therapy because she understood which exercises she needed to do throughout her recovery due to her previous surgical experiences. She started walking daily around her neighborhood, and within three weeks time, she was back to walking four miles per day. “I would recommend this surgery to anybody!” Now enjoys doing activities like Zumba, which she was never able to do before, and she’s thinking of trying some yoga in the near future.


 Many people enter the new year already dealing with lingering neck or back pain and simply learn to live with it. Pain that lasts longer than a few weeks, continues to return, or interferes with daily activities is not normal and should be evaluated.
Many people enter the new year already dealing with lingering neck or back pain and simply learn to live with it. Pain that lasts longer than a few weeks, continues to return, or interferes with daily activities is not normal and should be evaluated.
 246 Beatty Drive, Suite 100
246 Beatty Drive, Suite 100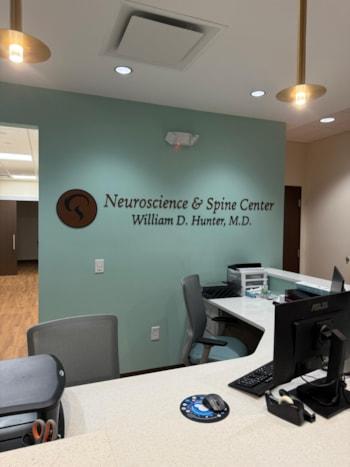 Under the leadership of
Under the leadership of  We look forward to welcoming patients to our new Belmont office in January 2026.
We look forward to welcoming patients to our new Belmont office in January 2026.